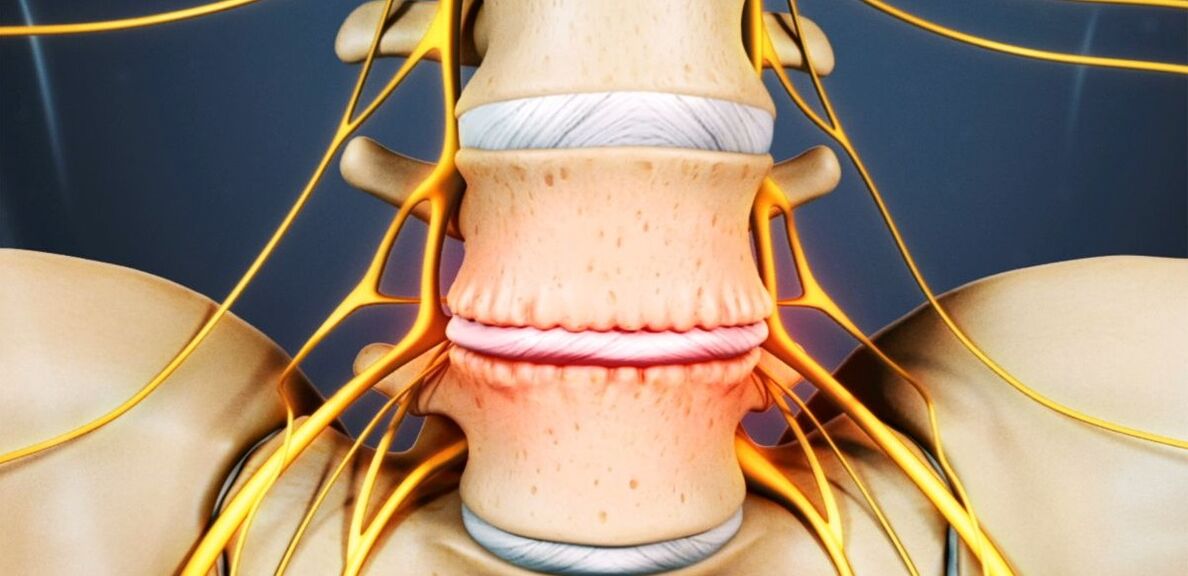
Osteochondrosis is a chronic degenerative-dystrophic disease that develops under the influence of many, quite disparate factors. Initially, pathological changes occur in the nucleus pulposus (the inner contents of the intervertebral disc), then they spread to the annulus fibrosus (the outer shell of the disc) and other elements of the spinal motion segment (SDS). This can be a consequence of the body's natural aging process, or it can occur against the background of injuries, increased loads on the spine and other causes. In any case, osteochondrosis is only the first stage in the destruction of the intervertebral disc, and if left untreated, protrusions and hernias are formed, which often require surgical removal.
The intervertebral disc is a formation of cartilage that separates the vertebral bodies and acts as a shock absorber.
Lumbar osteochondrosis: what is it
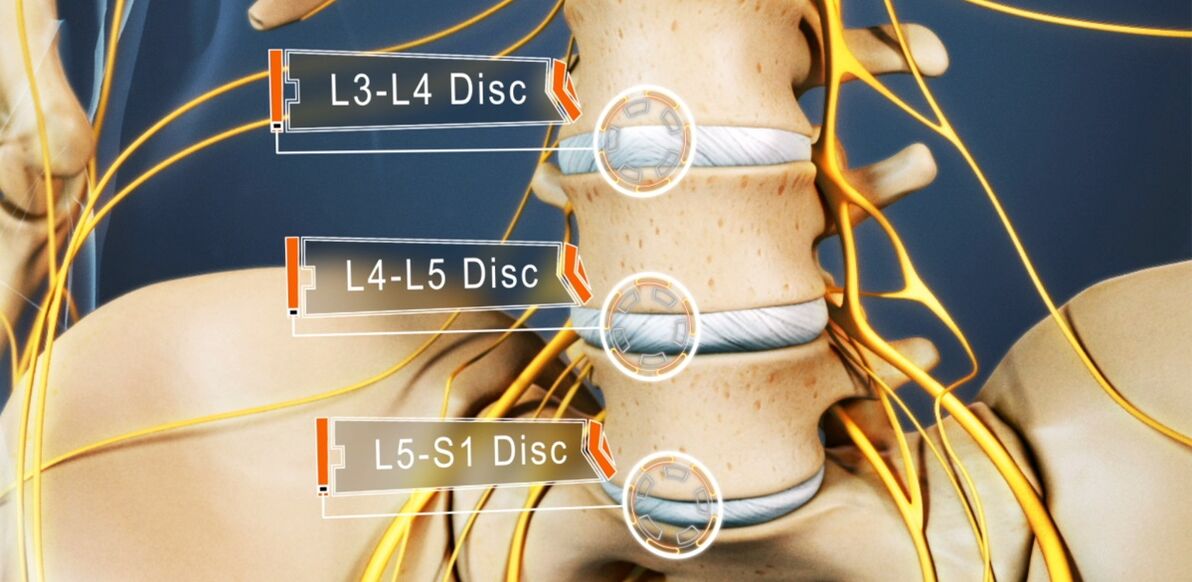
From osteochondrosis suffers from 48-52% of people. And osteochondrosis of the lumbar spine is the most common. The disease can affect any of the intervertebral discs of the lumbosacral spine, several of them, or even all of them. Most often, L5-S1, L4-L5 discs suffer, less often L3-L4. The upper lumbar discs (L3-L2 and L2-L1) are much less affected.
The prevalence of lumbar osteochondrosis is due to the fact that the greatest load in the performance of any physical work, in particular, lifting and carrying weights, walking, running, sitting falls on the lower back. The lumbar spine is made up of 5 vertebrae, much larger than the thoracic and cervical vertebrae. As a result, the intervertebral discs between them are larger in size. Normally, the lumbar region has a slight anterior curvature (physiological lordosis). It is the last moving part of the spine and is adjacent to the fixed sacrum, so it is most often referred to as lumbosacral osteochondrosis.
If earlier osteochondrosis was considered an age-related disease, today its first manifestations can be observed already at the age of 15-19. Among thirty-somethings, already 1. 1% of people suffer from severe symptoms of degenerative-dystrophic changes in intervertebral discs. And in representatives of the older age group (from 59 years), clinical manifestations of the disease are already present in 82. 5%. At the same time, the incidence of pathology continues to grow steadily, which is largely due not only to an increase in the average age of the country's population, but also to lifestyle changes that are notfor the best.
Reasons for development
Today, there is still no consensus on the etiology of degenerative diseases of the spine. Nevertheless, the main theory of their development is involutive. According to her, osteochondrosis is a consequence of previous damage to the intervertebral disc and bone structures of the spine, as well as the appearance of inflammatory and other processes. The theory suggests that degenerative changes are genetically predetermined and, in fact, inevitable. And their clinical manifestation, especially in young and middle-aged people, is due to the influence of various endogenous and exogenous factors.
Thus, the development of osteochondrosis of the lumbar spine is facilitated by:
- heavy physical labor, especially associated with lifting heavy loads;
- sedentary and sedentary lifestyle;
- any back injuries, including bruises;
- Overweight;
- Metabolic disorders;
- violations of posture, deformation of the spine;
- flat feet and other foot conditions;
- pregnancy, especially multiple pregnancy.

Pathogenesis
Whatever the causes, the degeneration of the intervertebral disc occurs when the intensity of the processes of catabolism (cleavage and oxidation of molecules) of matrix proteins begins to exceed the speed of their formation. One of the key points in this process is the malnutrition of the intervertebral discs.
Since they, like most cartilage in an adult, have no direct blood supply, as they lack blood vessels, the supply of nutrients and removal of metabolic products occurs by diffusion with compression and relaxationsequences of the disc during movement. The main structure that powers the disk consists of the end plates located on its upper and lower surfaces.
On their own, the endplates are a bilayer formed of cartilage cells and bone tissue. Accordingly, the cartilaginous side they are adjacent to the disc, and the bone - to the vertebral bodies. They are distinguished by sufficiently good permeability, which ensures the exchange of substances between cells, the intercellular substance of the disc and the blood vessels passing through the vertebral bodies. Over the years, especially with the negative impact of external and internal factors, the structure of the vertebral endplates changes and their blood supply decreases, which leads to a decrease in the intensity of metabolism in the intervertebral disc. As a result, its ability to produce new matrix is reduced, which leads to a gradual decrease in its density with age.
At the molecular level, this is accompanied by:
- a decrease in the rate of diffusion of nutrients and metabolic products;
- decreased cell viability;
- accumulation of cellular breakdown products and altered matrix molecules;
- a decrease in the production of proteoglycans (high molecular weight compounds responsible for the formation of new cartilage cells and which are the main sources of chondroitin sulphate synthesis);
- damage to the collagen scaffold.
Possible consequences
As a result of ongoing changes, the intervertebral disc is dehydrated, and the nucleus pulposus loses its ability to properly distribute the loads on it. As a result, the pressure inside the disc becomes uneven, and as a result, the annulus fibrosus in several places experiences overload and compression. As happens with every movement of a person, the ring is regularly subjected to mechanical pressure. This leads to unfavorable changes in it.
In addition, a decrease in disc height and elasticity often results in compensatory changes in the adjacent vertebral bodies. Bony growths called osteophytes form on their surface. They tend to increase in size over time and even merge with each other, excluding the possibility of movements in the affected PDS.
Due to the fact that malnutrition causes damage to the collagen skeleton, under the influence of the pressure of the nucleus pulposus in certain places, the normal structure of the fibers forming the fibrous ring is disturbed. Left unchecked, this eventually leads to cracks and breaks. Gradually, more and more fibers of the fibrous ring at the site of application of pressure are torn, which leads to its protrusion. This is especially facilitated by increased loads on the spine. And since the lumbar region bears the main load during movement and any physical activity, it most often suffers from it.
The protrusion of the intervertebral disc without a permanent rupture of the fibrous ring and with the size of its base greater than the protruding part is called a protrusion. With its complete rupture in one place or another, an intervertebral hernia is diagnosed.
With the destruction of part of the fibers of the fibrous ring, the pressure in the disc gradually decreases, which leads to a decrease in tension and in the fibers themselves. This leads to a violation of its fixation and, as a result, to pathological mobility of the affected spinal motion segment.
The vertebral motor segment (SMS) is a structural and functional unit of the spine formed by the intervertebral disc, the adjacent vertebral bodies, their articular facets, the ligaments and the muscles attached to these bony structures.
Normal functioning of the spine is only possible with proper functioning of the PDS.
Symptoms of osteochondrosis of the lumbar spine
The disease can be asymptomatic for a long time, then begin to manifest itself as mild discomfort in the lumbar region, gradually gaining strength. But in some cases, lumbar osteochondrosis begins acutely, immediately causing a powerful pain syndrome. In most cases, the first signs of pathology appear after 35 years.
Back pain is the main symptom of the disease. It can be of different character and be both painful and dull, and sharp, constant or episodic. But fundamentally for pathology, especially in the early stages of development, the alternation of periods of exacerbation and remission is characteristic, and hypothermia or lifting a heavy object, or a sharp unsuccessful movement can causea further deterioration in well-being.
The pain is often accompanied by a feeling of numbness and tension in the back muscles. They are aggravated by physical exertion, sudden movements, heavy lifting, bending, and even coughing and sneezing.

If, due to the instability of the vertebral bodies, the nerve root extending from the spinal cord is pinched by one or another anatomical structure, this will lead to the development of appropriate neurological disorders. Their main manifestations are:
- stitches, severe pains radiating to the sacrum, buttocks, lower limbs or perineum;
- sensitivity disorders of varying severity;
- mobility restrictions, lameness;
- weakness of the muscles innervated by the pinched nerve.
In the lumbar spine, the spinal cord ends at the level of 1-2 vertebrae and passes into the so-called ponytail, formed by an accumulation of vertebral roots. Moreover, each of them is responsible not only for the innervation of muscles, but also of specific organs of the small pelvis, so prolonged compression can disrupt the work of the corresponding organ. This can lead to the development of impotence, infertility, gynecological diseases, hemorrhoids and other disorders.
The clinical picture of osteochondrosis of the lumbar spine, especially with a long course and the occurrence of compression of the vertebral roots, largely depends on the level of the lesion, that is, on the particular disc thathas undergone degenerative-dystrophic changes.
- The defeat of the L3-L4 disc - the pain is given to the antero-internal parts of the thigh, lower leg and inner ankle. This is accompanied by a decrease in the sensitivity of the front side of the thigh, a decrease in the severity or loss of the patellar reflex, as well as a decrease in the strength of the quadriceps muscle.
- The defeat of the L4-L5 disc - the pain is given from the upper part of the buttocks to the outer parts of the thigh and lower leg. Less commonly, this is accompanied by pain spreading to the back of the feet, including 1 to 3 fingers. In these areas there is a decrease in tenderness and muscle weakness. Sometimes hypotrophy and incomplete extension of the big toe develop.
- L5-S1 disc damage - pain begins in the midline area of the buttocks and travels down to the heel along the posterior or posterior surface of the thigh and lower leg and may capture the outer edge of the foot, as 4-5 fingers. In these areas of the lower extremities there is a decrease in sensitivity, and the gastrocnemius and gluteus maximus often decrease in size, which is accompanied by their weakness. If the spinal root passing through this PDS is affected, a decrease or loss of ankle and plantar reflexes may be observed.
The L1-L2 and L2-L3 discs are rarely affected.
The pain that accompanies the disease restricts a person and significantly reduces the quality of his life. Since they persist for a long time and recur regularly, if not constantly present, this cannot but affect the psycho-emotional state. As a result, more than half of patients show signs of chronic emotional stress, depressive disorders, etc.
Diagnostic
If there are signs of osteochondrosis of the lumbar spine, you should contact a neurologist or vertebrologist. First of all, the doctor collects an anamnesis, which consists in clarifying the nature of the complaints, the features of the pain, the conditions of their occurrence and reduction, the features of a person's professional life, etc.
The second stage of diagnosis, carried out as part of the first consultation with a doctor, is a physical examination. During it, the doctor assesses the condition of the skin, posture, the depth of the physiological curves of the spine, the presence of its curvature, etc. The condition of the muscles surrounding the spine, called paravertebrals, is necessarily assessed, since they are often sore and overly tense, which is a reflex reaction of the body to inflammation and discogenic pain.
Already on the basis of the data obtained during the examination and questioning of the patient, the neurologist can suspect the presence of osteochondrosis of the lumbar spine. But to exclude possible concomitant pathologies, as well as to confirm the diagnosis and accurately determine the level of damage, the severity of degenerative-dystrophic changes in the intervertebral disc and the involvement of bone structures, laboratory and instrumental diagnostic methodsare necessary.

Laboratory diagnosis
Analyzes of various kinds are not decisive in the diagnosis of osteochondrosis of the lumbar spine. They are aimed more at assessing the degree of the inflammatory process and detecting concomitant disorders.
Thus, they can be affected:
- UAC;
- OAM;
- blood test for sugar level;
- blood chemistry.
Instrumental diagnosis
All patients with suspected osteochondrosis of the lumbar spine have:
- x-ray of the lumbar spine in two projections - allows you to determine the structure of bone structures, detect anomalies, formed osteophytes, changes in facet joints, etc. ;
- CT - allows you to detect changes in bone structures at earlier stages of development than X-rays, as well as identify indirect signs of osteochondrosis;
- MRI is the best method for diagnosing pathological changes in cartilaginous formations and other soft tissue structures, which makes it possible to detect the slightest changes in the intervertebral discs, ligaments, blood vessels and spinal cord andaccurately assess their severity and potential risks.

In addition, it may be recommended to:
- densitometry - a method of determining bone density, which allows to diagnose osteoporosis, which is especially common in the elderly;
- myelography - allows you to assess the condition of the CSF pathways of the spinal cord and the degree of damage to the protruding disc, which is especially important in the presence of an already formed intervertebral hernia of the lumbar spine.
Treatment of lumbar osteochondrosis
When diagnosing osteochondrosis, as a rule, all patients are initially prescribed conservative treatment, provided that there is no pronounced and progressive neurological deficit. But his character is selected strictly individually.
Since the disease is chronic and the regenerative abilities of the intervertebral discs are extremely limited, especially with pronounced degenerative-dystrophic changes, the main goals of treatment are to stop their further progression and eliminate the symptoms that disturbthe patient. Therefore, treatment is always complex and includes:
- drug therapy;
- manual therapy;
- physiotherapy;
- exercise therapy.
In the acute period, patients have been shown to limit physical activity or even adhere to bed rest for 1-2 days. This will help relax the muscles and reduce the pressure inside the disc. If you have to sit, walk or do physical labor for a long time, you should wear a lumbar stabilizer corset.

After the end of the acute period and during the remission of the disease, on the contrary, it is important to move as much as possible, but with caution and excluding increased stress on the lower back. Patients will need to acquire the necessary skills to sit correctly, lift objects from the floor, carry heavy loads, since all this affects the course of the pathology. It is important to avoid inclinations and sudden movements, to lift something from the floor or low surfaces, after bending the knees and not to bend over. You should only sit with your back straight in a chair that supports your back well. In addition, during sedentary work, it is important to regularly take breaks for a short workout. It is important to avoid falls, jumps, rapid running and hypothermia.
With osteochondrosis, it is important to maintain body weight within optimal limits, and with obesity, diet and physical exercises appropriate to the patient's condition are indicated, since excess weight creates an increased loadon the lower back and causes a faster progression of pathological changes in the discs.
On average, conservative treatment is usually designed for 1-3 months, although it can last longer. But even after completing the main course prescribed by the doctor, it will be necessary to continue taking a number of medications, carrying out therapy and following lifestyle recommendations.
medical therapy
The main components of drug therapy are individually selected drugs from the group of NSAIDs. When choosing them, the doctor takes into account not only the severity of the pain syndrome and the course of the inflammatory process, but also the nature of concomitant diseases, especially of the digestive tract, since NSAIDs with prolonged use can adversely affectthe condition of their mucous membranes and cause an exacerbation of various pathologies of the digestive system.
It is necessary to use NSAIDs for acute pain in the lower back and immediately after it appears. Preferably in 1-2 days. Depending on the severity of the patient's condition, they can be administered intramuscularly, in the form of rectal suppositories, local agents and in oral form. The duration of admission should not exceed 2 weeks. In the future, an individually selected drug is taken on demand, but trying to avoid frequent use.
Recently, preference is more often given to drugs, as an active ingredient, which include selective inhibitors of cyclooxygenase-2.
Also, patients are prescribed drugs from the following groups:
- muscle relaxants - help relax over-tightened muscles and thus reduce back pain;
- chondroprotectors - improve the course of metabolic processes in the intervertebral disc (especially effective when started in the early stages of development of lumbar osteochondrosis);
- B vitamins - contribute to the improvement of nerve conduction;
- antidepressants and anxiolytics - used for long-term osteochondrosis, which led to depression, chronic fatigue and other psychological disorders.
With very severe pain, especially of neurological origin, therapeutic blockades are performed. They involve the introduction of anesthetics in combination with corticosteroids at points near the compressed nerve, which leads to the rapid elimination of pain. But the procedure can only be performed in a medical facility by specially trained health workers, as it is associated with the risk of complications.
Manual therapy
Manual therapy allows not only to improve the quality of blood circulation in the zone of influence, but also to significantly reduce the severity and duration of pain in osteochondrosis. It effectively relieves muscle tension and allows you to eliminate functional blockages, which significantly increases mobility in the affected SMS.
In addition, with properly conducted manual therapy, it is possible not only to increase the distance between the vertebrae, return them to their anatomically correct position, but also to release the compressed nerve roots. As a result, pain is quickly eliminated and neurological disorders disappear. It also reduces the risk of complications and disturbances in the work of internal organs.

The additional positive properties of manual therapy improve mood, boost immunity, activate the body's natural recovery mechanisms and increase efficiency. Usually after the 1st session there is a noticeable improvement in well-being, and in the future the effect becomes more pronounced. As a rule, the course consists of 8-15 sessions, and it is important to complete it to the end, even with complete normalization of well-being.
Physiotherapy
After the disappearance of acute inflammation, courses of physiotherapeutic procedures are indicated, which not only help to reduce pain, but also improve microcirculation, nutrition and the course of repair processes in the area of degenerative-dystrophic changes. Most often, patients are prescribed:
- electrophoresis with the introduction of drugs;
- electrical neuromyostimulation;
- ultrasound therapy;
- laser therapy;
- magnetic therapy;
- UHF.
Which specific methods of physiotherapy will give the best effect, the frequency of their implementation, the duration of the course and the possibility of combining with other types of exposure are determined individually for each patient.

Traction therapy gives very good results in osteochondrosis of the lumbar spine. Thanks to this, it is possible to increase the distance between the vertebral bodies, which instantly reduces the load on the affected discs. After the session, to consolidate the results, the patient must wear an orthopedic corset.
exercise therapy
After the elimination of acute pain, the treatment program is necessarily supplemented with exercise therapy. Its main tasks are to stretch the spine and relax the spasmodic muscles of the lower back. In addition, therapeutic exercises help strengthen the muscle corset, create reliable support for the spine and improve posture. During this, blood circulation is inevitably activated and metabolic processes are improved, which has a beneficial effect on the nutrition of discs.
For each patient, a set of exercises is selected individually depending on the degree of degenerative-dystrophic changes, the level of physical development of the patient, the nature of concomitant disorders, age and other factors. Initially, it is recommended to study under the guidance of an experienced exercise therapy instructor.
All patients with degenerative changes in the spine are recommended to visit the pool 2-3 times a week, since swimming lessons minimize the load on the spine, but allow you to effectively strengthen the muscles of the back.
Thus, osteochondrosis of the lumbar spine is one of the most common diseases. At the same time, it can deprive a person of his ability to work for a long time and even lead to disability due to the development of complications. Therefore, it is important not to ignore the first symptoms of the disease, when it is easier to manage. With the appearance of pain, and even more so numbness, reduced mobility, back pain, you need to contact a neurologist as soon as possible, undergo the necessary examination and begin treatment. In this case, it will be possible to stop the pathological process and return to a normal, full life without pain and significant restrictions.

























